Per the Diabetes Atlas, over 40,000 people in South Africa suffer from diabetes. And, according to the Type 1 Diabetes Index, 39 healthy South African lives are lost due to the condition. What’s more, an estimated 100,000 people are undiagnosed, according to the Diabetes Atlas. Here’s what to know about Type 1 diabetes specifically.
What Is Type 1 Diabetes?
Type 1 diabetes is a chronic autoimmune condition in which the pancreas produces little to no insulin. It is provoked by an autoimmune reaction, in which the body attacks the cells in the pancreas that produce insulin. Without insulin, glucose builds up in the bloodstream and cannot enter cells to produce energy, leading to elevated blood glucose levels and a range of symptoms and potential complications.
This process may unfold for months or years before symptoms appear. While some individuals with type 1 diabetes have a genetic predisposition to the condition, others do not, and researchers are still working to pinpoint potential environmental factors—like viruses or other stressors—that may trigger the autoimmune attack. Diet and lifestyle habits do not cause type 1 diabetes.
Type 1 diabetes has historically been referred to as “juvenile” or “insulin-dependent” diabetes. But Dr Joel Zonzsein, director of the Diabetes Center at the University Hospital of the Albert Einstein College of Medicine, notes that although the condition is “mostly diagnosed in children and young adults, it can develop at any age and should be taken seriously as a possibility in adults—referred to in such cases as ‘latent autoimmune diabetes of the adult’ (LADA).”
What Are The Causes Of Type 1 Diabetes?
Type 1 diabetes is caused by an autoimmune reaction. Having a parent or sibling with the disease may increase your risk for developing type 1 diabetes. Environmental factors may also play a role in triggering the autoimmune reaction, but researchers are still working to better understand this possible pattern.
What Are The Symptoms Of Type 1 Diabetes?
Type 1 diabetes symptoms may occur suddenly, often in adolescence or early adulthood and can include:
Talk to your healthcare provider if you notice any of the above symptoms in yourself or your child. In some cases, the first noticeable symptoms of type 1 diabetes may be signs of a life-threatening state called diabetic ketoacidosis (DKA). Symptoms of DKA include:
If you or your child have symptoms of DKA, contact your doctor or go to the nearest emergency room immediately.
How Is It Diagnosed?
Diagnosing type 1 diabetes requires only a few simple tests. Doctors most often use a random plasma glucose (RPG) test, which measures blood glucose at a single point in time, to diagnose. A random blood-glucose test higher than 200 mg/dL suggests a diabetes diagnosis, regardless of when you last ate a meal or snack. Often, a healthcare provider will use an A1C blood test, which provides an average of blood glucose levels over a period of three months, to determine the duration of a patient’s high blood glucose.
While these tests can determine whether you have diabetes, they cannot differentiate between type 1 and type 2 diabetes. Treatment plans differ significantly between the two conditions, so it is crucial to have a correct diagnosis.
To determine if you have type 1, a doctor will test the blood for specific auto-antibodies that are a common marker of the autoimmune reaction that causes the condition. They may also test your urine for ketones, which are produced when the body burns fat for energy instead of glucose and indicate type 1 diabetes if present.
How Is Type 1 Diabetes Treated?
While treatment options have significantly advanced in the past few decades, there is no cure for type 1 diabetes. So living with it—and preventing later complications—requires close blood-glucose management, via a blood-glucose meter or a continuous glucose monitor.
Type 1 diabetes is primarily managed via insulin therapy. Different types of insulin work at different speeds and last different lengths of time. You may need to use more than one type. Insulin can be taken in several different forms to best suit personal preferences and lifestyles:
- Syringes and pens: These are injected multiple times daily and often involve a combination of short- and long-acting insulin types. Different brands vary slightly in their effective onset, peak time and duration.
- Insulin pumps: Pumps are small devices that deliver a continuous supply of long-acting insulin throughout the day via a small tube inserted under the skin, mimicking a healthy pancreas. They can also be programmed by the user to release short-acting insulin during mealtimes.
- Artificial pancreas (AP) systems: These systems combine the functions of an insulin pump with a continuous glucose monitor to adjust insulin delivery based on glucose fluctuations. By responding to real-time glucose readings, AP systems can regulate blood sugar more effectively than traditional manual methods. As the name indicates, this form of closed-loop management most effectively imitates a healthy pancreas—but does require the use of two devices at all times.
- Inhaled insulin: Quick-acting inhaled insulin is one of the newer forms of FDA-approved treatment for type 1 diabetes management. It is used in combination with long-acting insulin (either via injection or pump) and inhaled shortly before meal times. However, according to Diabetes South Africa, this treatment is not yet available here.
Living With The Condition
Living a healthy life with type 1 diabetes also involves lifestyle adjustments, including:
- Regular blood-glucose monitoring: Checking blood-glucose levels throughout the day is essential to managing the condition and preventing future complications that can result from prolonged high blood sugar.
- Carbohydrate counting: In order to maintain stable blood-sugar levels, it’s often important to match your insulin dosage to your carbohydrate intake. An endocrinologist can help you determine your individual insulin-to-carb ratio and dose accordingly for each meal and snack. Managing this condition does not require you to give up your favourite foods—so long as you know how to dose for them!
- Movement: Regular exercise can help to regulate blood sugar levels and improve long-term health.
- Regular checkups: People living with type 1 diabetes should regularly meet with a team of medical specialists, including an endocrinologist, optometrist and in some cases a dietitian, to help monitor their blood-glucose management and prevent future complications.
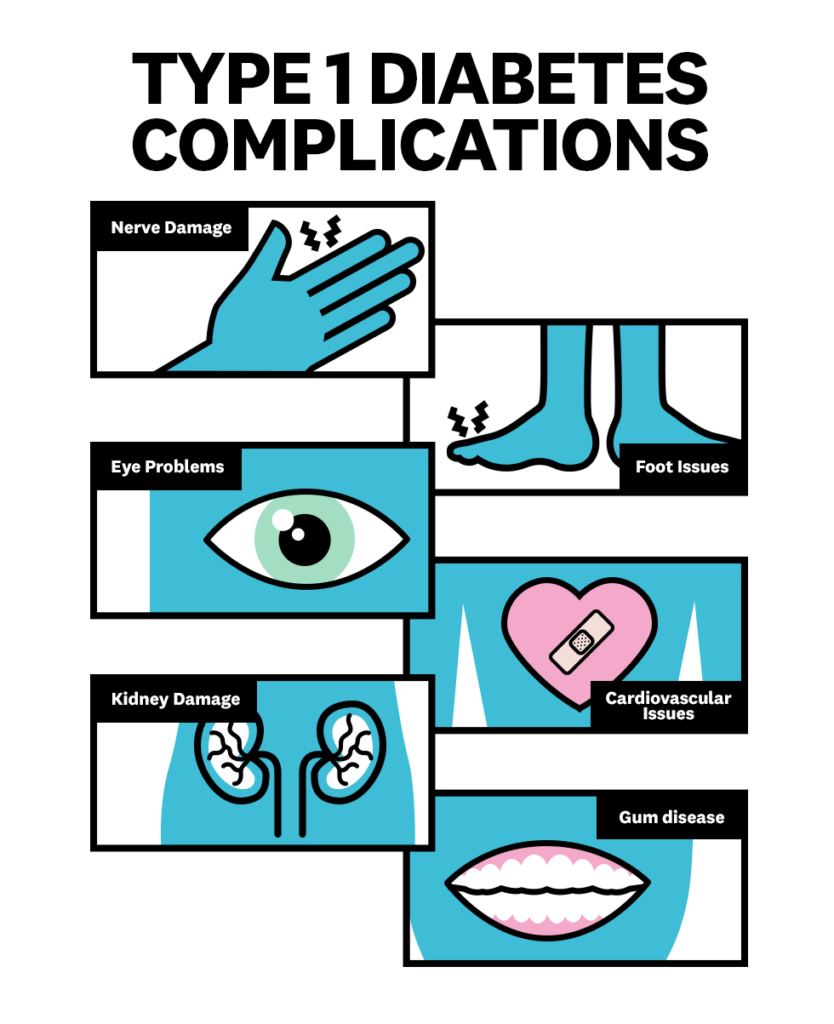
Complications Of Type 1 Diabetes

Although this is a chronic and lifelong condition, many people live long and healthy lives with it, with few or no associated complications. “Keeping blood sugar levels under control is the most important thing that people with type 1 diabetes can do to prevent complications,” Dr Zonszein says. He also emphasises the importance of regular check-ups and developing a good management plan with a team of medical specialists.
Poorly managed type 1 diabetes—namely, continuous high blood sugar, or hyperglycemia—can damage several areas of the body. Complications can include:
- Nerve damage: Prolonged high blood glucose levels can cause nerve damage. This leads to diabetic neuropathy, which most often affects the hands and feet.
- Eye problems: Elevated or uncontrolled blood glucose levels can also cause diabetes-related retinopathy. This can lead to vision loss, blindness, macular oedema and glaucoma.
- Kidney damage: High levels of glucose in the blood can damage the blood vessels and filters in the kidneys (nephropathy).
- Foot issues: High blood glucose levels can reduce the blood supply to the feet, resulting in reduced sensation. This can increase the risk of wounds, cuts, infections and non-healing sores.
- Complications related to the heart and blood vessels: Extended high blood glucose levels can damage the blood vessels and nerves. It can increase your risk of heart attack, stroke and high blood pressure.
- Gum disease: Excess glucose in the blood can move into the saliva, causing germs and plaque. These increase the risk of tooth decay and gum disease.
How To Prevent It
Unfortunately, there is no way to prevent type 1 diabetes. Because it can be passed down genetically, your family can be preemptively tested for auto-antibodies. Their presence in the blood—even in the absence of symptoms—can help catch the early onset of the condition.
This story was written by Zoë Brown and was first published on WomensHealthMag.com
Adblock test (Why?)
Powered by WPeMatico